How Unregulated Antifungal Creams Are Driving India's Ringworm Epidemic
A curable fungal infection has turned into a silent epidemic in India, driven by irrational steroid–antifungal creams, poor regulation, and structural neglect. This photostory traces how a simple itch spirals into chronic illness, resistance, and quiet suffering among the poor.
A Mere Itch
Daad, dinai, khujli, daadar, jaadu—names that echo across homes in Jharkhand, Bihar, Gujarat, and Odisha—are all terms for what medicine calls ringworm or tinea.
Once considered seasonal, this common fungal infection now persists year-round, thriving in crowded homes, hard labour, limited water, poor nutrition, and unequal access to care, quietly becoming endemic among the poor.
This photo shows widespread fungal infection of the skin affecting various body parts from a woman in Orissa.
Missed Diagnoses
Diagnosis is often the first weak link in the care of fungal infections in rural areas.
In overstretched clinics and informal settings, ringworm is frequently diagnosed by sight alone, with little attention to clinical nuance or alternative possibilities.
This has real consequences: this is a picture of a woman with leprosy in Bihar who was treated for months as having a fungal infection, her disease masked and altered by irrational steroid-based creams.
Avoidable Suffering
While fungal cultures are slow, expensive, and rarely available in the very regions where disease burden is highest, a simple and inexpensive test—10% KOH microscopy of skin scrapings—can detect fungal elements in nearly 80% of cases when done well.
Yet this basic outpatient diagnostic skill is disappearing. The erosion of clinical acumen, combined with the neglect of simple microscopy, has normalised blind treatment, delayed correct diagnoses, and prolonged avoidable suffering.
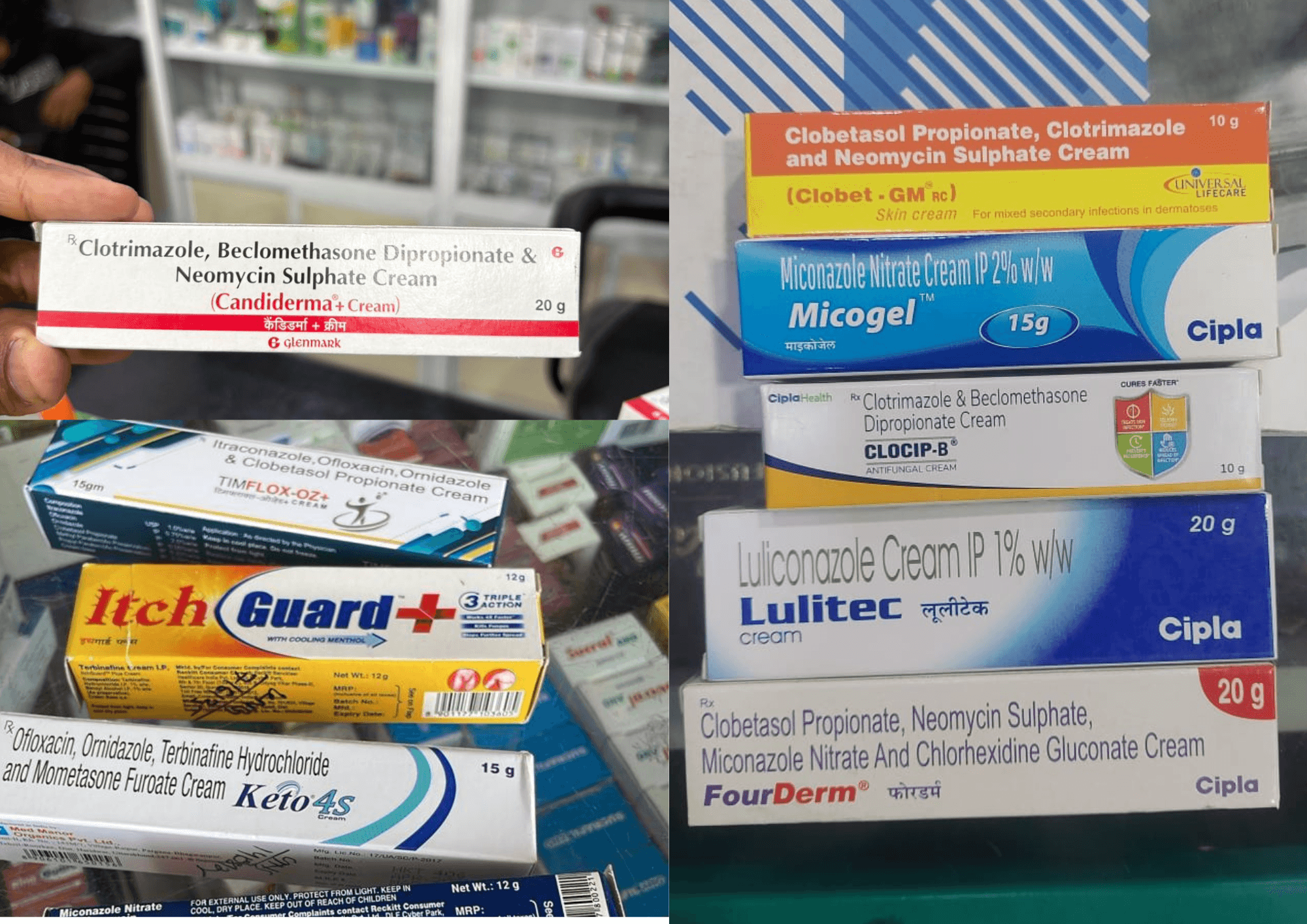
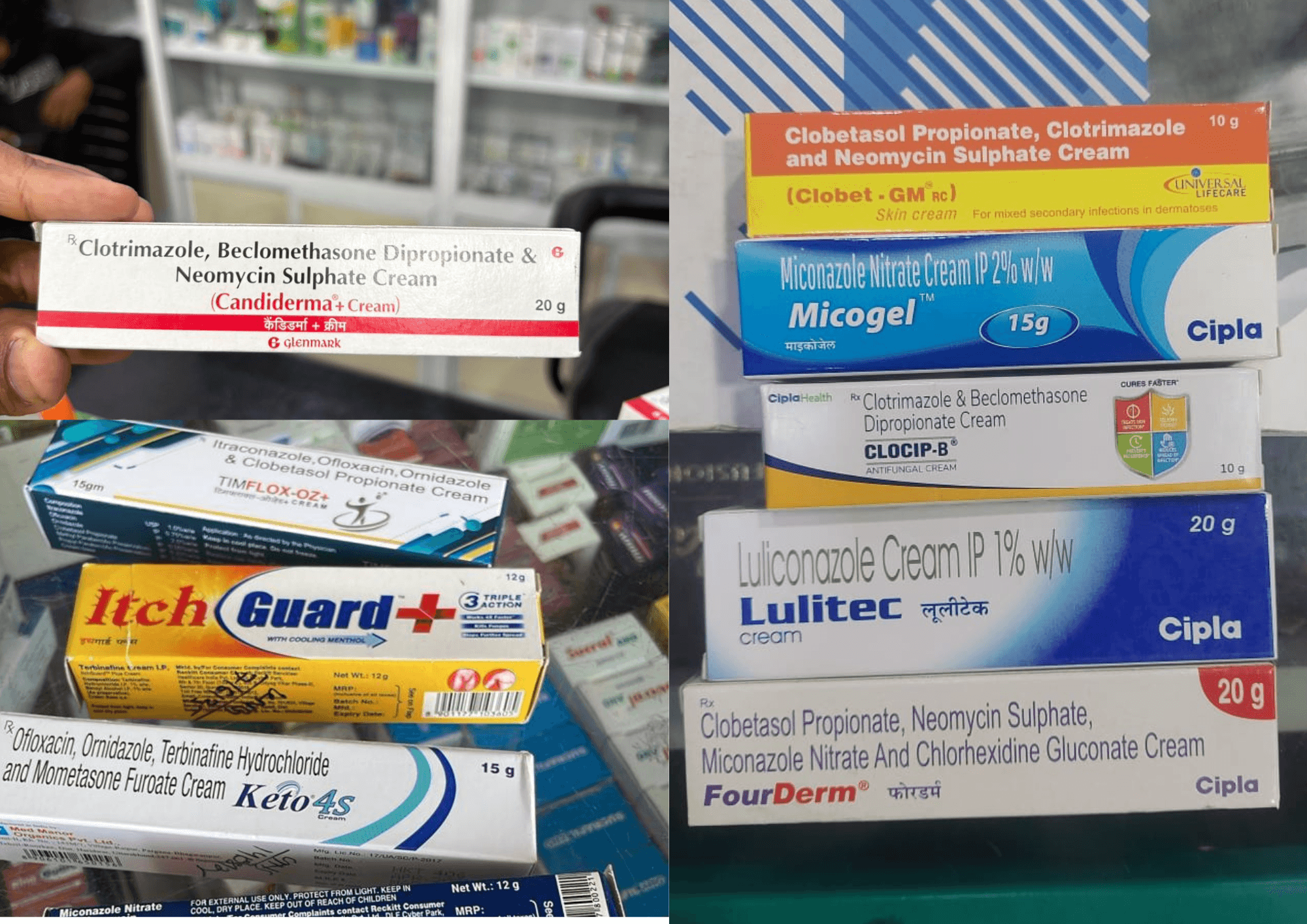
A Market Built on Misdiagnosis
In the face of weak diagnostic capacity and eroding clinical acumen, the pharmaceutical response has not been to strengthen diagnosis but to bypass it.
The market is now flooded with irrational combination creams that bundle an antifungal with a potent steroid and an antibiotic—designed to “cover all bases” when clinicians or practitioners cannot, or do not, make a precise diagnosis.
These combinations offer quick symptomatic relief, especially from itching, masking disease rather than curing it. In reality, steroids and antibiotics are rarely indicated in fungal infections, and when they are, they should be prescribed separately and with clear justification.
This strategy of overtreatment has fuelled the rise of chronic, widespread, and difficult-to-treat infections, turning a once simple condition into a growing public health problem.
This image shows a few combinations available at a Delhi pharmacy. (Photo credits for this image: Sayan)
When the author Vasundharaa asked the pharmacist in Delhi, she was told they have around 80 different formulations available as different doctors have different brand preferences.
Dr Yogesh Marfatia, a former professor of dermatology at Vadodara Medical College and the past national president of the Indian Association of Dermatologists and editor of IJDVL journal, says that over the years, many people had written letters to drug regulators about these combinations, but not much was done about it.
He says that even when some antifungal combinations get banned, pharmaceutical companies push new ones into the market.
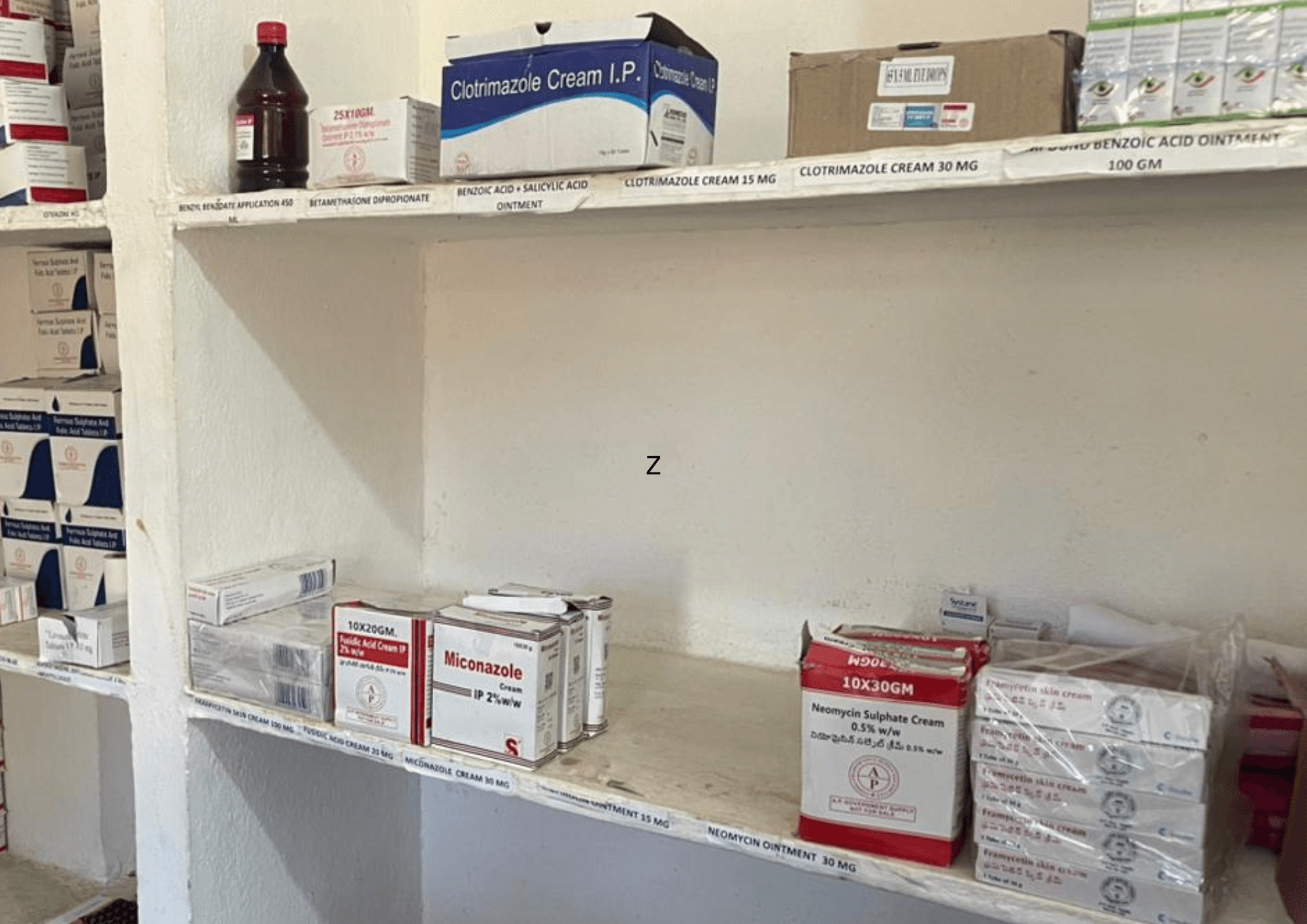
Unchecked, Everywhere
Antifungal creams, which were once meant to be regulated drugs, are now ubiquitous across the country, available over the counter in pharmacies large and small, from cities to remote towns.
Many are sold in these unapproved, irrational combinations, their steroid component offering quick relief from itching while quietly worsening the disease. Patients, reassured by temporary comfort, are caught in a cycle of misuse and recurrence.
In 2023, India’s antifungal market crossed USD 700 million and is projected to reach USD 1 billion soon, driven largely by superficial antifungal ointments. This explosive growth reflects not better care, but widespread overuse and weak regulation.
The pictures here show antifungal creams from Kerala, Odisha and Chennai. Of these, only Chennai creams needed prescription for buying. (Photo credits for image from Chennai: Sankalpa)
When the author Vasundharaa asked a Gujarat pharmacist which drug do they stock the most, she was shown a very expensive combination, costing around Rs 300 per tube - saying this is what most doctors prefer.

Terrible Consequences
This patient from Surguja, Chhattisgarh, has been on treatment for his fungal infection for more than a year without resolution.
The patient has been spending around 6000 - 7000 Rs per month on his treatment, and had to drive a bike for more than an hour regularly to seek care.
After long-term treatment with steroids, he has now developed various side effects of steroids, including facial puffiness known as moon facies. He also had severe weakness, bone and muscle pain, along with depressive symptoms.
Alongside losing money, patients also suffer from emotional distress, shame, frustration and sleep disturbances that occurs from recurrent long standing itching.
This is especially pronounced when the fungal infection is in the genital area and the patient is female or gender diverse.
Listen to the author's interview with this patient on this link
Furthermore, doctors are also seeing an increase in antibacterial and antifungal resistance due to such irrational prescription of drugs as evidenced by this paper, which says that the scale of this problem in India is unprecedented.
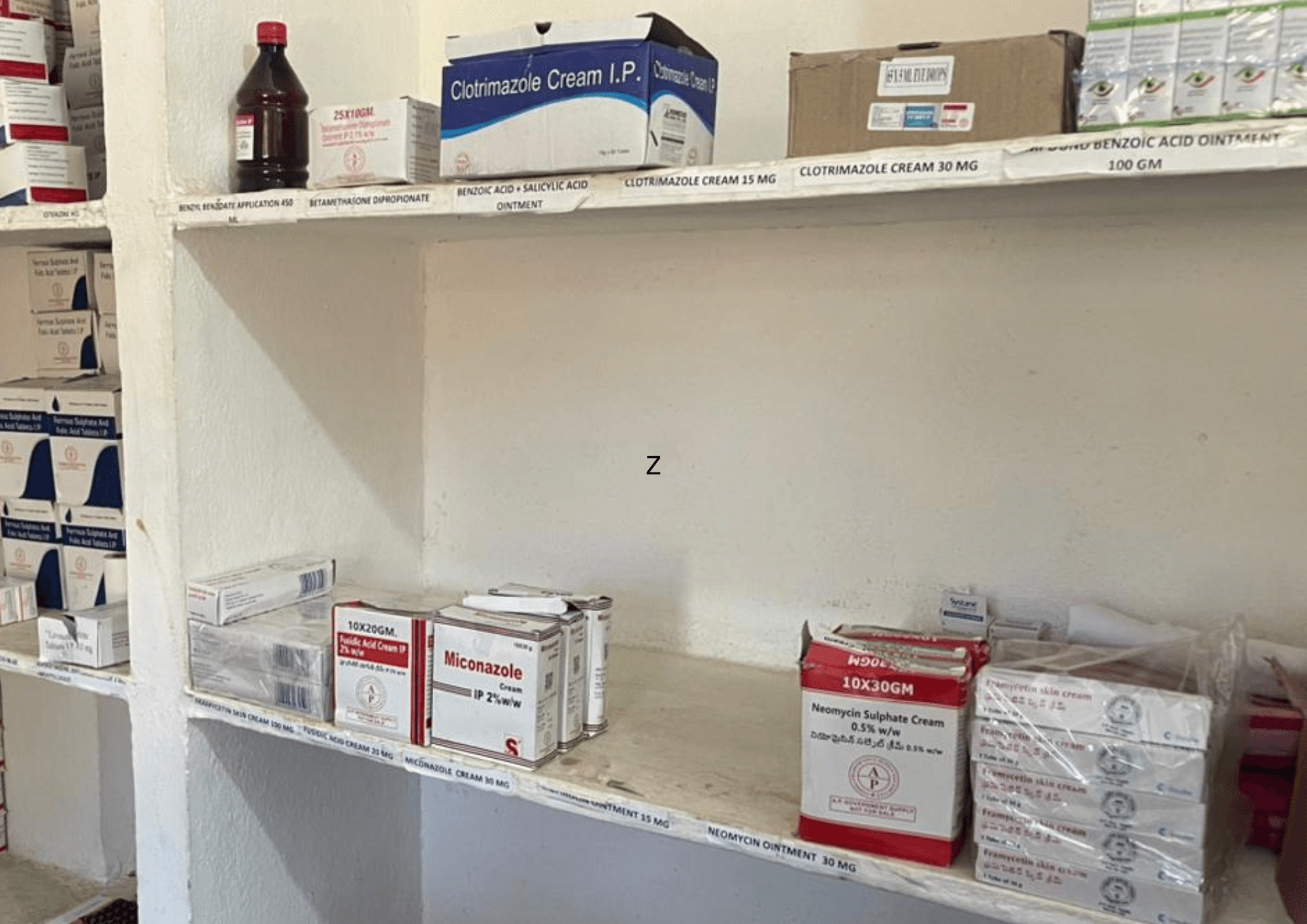
A Line Not Yet Crossed
Despite their ubiquity in private pharmacies, irrational antifungal combination creams have not fully penetrated government supply chains.
In public health facilities, including primary health centres in rural areas treatment still relies on separate, rational medications—plain antifungals prescribed on their own, with steroids or antibiotics used only when clearly indicated.
Allowing private-market logic to seep into these spaces would be disastrous
We must hold this line.
The photo shows a rural PHC in Paderu, Andhra Pradesh, stocking plain antifungal creams.
Regulation is a Moral Imperative
This crisis demands more than individual correction—it calls for systemic reform.
When a simple, curable infection is allowed to become chronic, deforming, and financially ruinous for the poor, the failure is moral as much as medical.
Weak regulation, permissive markets, neglected diagnostics, and the normalisation of irrational drugs together constitute structural violence against those with the least capacity to bear it.
Reform must mean enforcing drug regulation, strengthening diagnostic skills at the primary-care level, protecting public health supply chains from commercial capture, and centring care on cure rather than profit.
Anything less is a quiet acceptance of preventable suffering.
This is a picture of the lady with leprosy from Bihar after she finally recieved the correct diagnosis and treatment. A combination of good clinical acumen and a negative fungal microscopy saved her from longterm suffering from the disease, side effects of steroids, shame as well as several thousand rupees in out of pocket expenditure.
Her story illustrates why healthcare system reform must happen.
(Photo credits of this picture: Dr Abhitesh Tripathi, DNB Family Medicine, working in Gopalganj, Bihar)
Graphic by Christianez Ratna Kiruba