Diabetes is a growing global health challenge, affecting an estimated 53.7 crore adults worldwide in 2021 – a number expected to rise to 64.3 crore in 2030.
Diabetes is a disease caused by the inability of one’s pancreas to produce insulin – a hormone responsible for ensuring that one’s blood sugar remains in the normal range. The pancreas does this by allowing the sugar in the bloodstream to enter other body cells to be utilised as energy. Without insulin, blood sugar levels rise dangerously, leading to life-threatening complications.
While Type 2 Diabetes, usually seen in older adults, only requires insulin supplementation treatment as a last resort, Type 1 Diabetes, seen in children and younger adults, can be treated with only lifesaving insulin therapy.
Globally, about 9-10% of the adult population has diabetes, with India bearing a significant part of this burden. In India, 7.7 crore adults live with diabetes, including nearly 10 lakh people with Type 1 Diabetes who require insulin to survive. Alongside this, recent studies show that a significant proportion of Indian patients with Type 2 Diabetes also use insulin therapy for sugar control.
While Diabetes is a manageable condition when treated appropriately, insulin access and usage face significant challenges, particularly in resource-limited settings like India.
Insulin therapy demands not just the availability of the drug but also an infrastructure that supports its effective administration - such as a way to maintain the cold temperature needed for the insulin consistently and the ability to learn how to appropriately administer and adjust the doses needed for the patient on a day to day basis.
However, systemic barriers such as education, storage, logistics, and affordability create complex challenges for patients and healthcare providers alike. These hurdles often turn a treatable disease into a life-threatening condition, especially in rural and underserved areas.
Lack of Education as a Barrier to Treatment
When 13-year-old Swapnil came to Chinchpada Christian Hospital in a rural area of the Indian state of Maharashtra with a capillary blood sugar level three times higher than normal and severe abdominal pain, Ashita Singh, a doctor, diagnosed him with diabetic ketoacidosis. This is a life-threatening condition that develops when your body doesn't have enough insulin to allow blood sugar into your cells for use as energy, especially in Type 1 diabetes.
Swapnil’s health improved after the required treatment of insulin and intravenous fluids, but his doctors faced a new problem – Swapnil needed to continue taking insulin at home to keep his sugars in the normal range, and no member of his family was literate enough to read numbers.
Singh reflects on how to guide someone through the complex task of managing four different insulin doses with meals, especially when reading numbers is a significant challenge for them.
Swapnil was not the first patient with Type 1 diabetes mellitus who had come to Chinchpada Hospital with such a problem. “Over the years, I have faced challenges in dosing insulin for many of my patients with Type 1 diabetes because of their lack of education,” says Singh.
“Insulin dosing requires patients to understand some basic mathematics and perform basic calculations. It requires them sometimes to check their blood sugars and understand what those values mean,” says Singh.
She says what complicates the matter is the high stakes involved. “Overdosing might lead to fatally low blood sugar levels, and underdosing can lead to long-term complications.”
Singh and her medical team counter the problem by giving each patient insulin syringes with bright stickers indicating the point to which the syringes should be loaded. They also draw a sun or a moon on the stickers to indicate what time of day the syringe should be used. Many Indian doctors are doing the same thing for illiterate patients.
Logistical Challenges of Storing Insulin
Royson D’souza, a surgeon working in the hills of Gudalur at the Gudalur Ashwini Adivasi Hospital, says he knows of no Type 1 diabetics in the area who has survived past the age of 25.
Added to illiteracy is the problem of storage in rural areas, he says. Insulin must be stored in a cool, dark place — ideally in a refrigerator. But few people in rural areas own fridges. But even when they do, “many areas do not guarantee an uninterrupted power supply. These practicalities make maintaining the cold chain extremely difficult,” says D'souza.
“We teach them something called the double-pot method for storage,” says Manoj Dhinagar, a community health physician associated with Christian Medical College and Hospital, who practices in the villages surrounding the city of Vellore in Southern India, said over a telephone interview. The method involves storing insulin inside two clay pots, one inside the other. This helps to keep the insulin at a lower temperature than the external environment.
Only one study has explored low-resource cooling methods including clay pots and others options. While it found that these methods could lower storage temperatures by about eight degrees Celsius, it did not assess whether insulin stored this way remained effective.
Singh says these issues are further complicated by geographical access. Though many primary health centres exist, insulin is not stocked at them. It is mainly kept in district hospitals, which are often far away from patients who live in remote villages. On top of this, the lack of good public transport means patients might run out of insulin for several days before they can restock it.
“A lot of Type 1 diabetics are also sickly. Expecting them to make these long journeys to avail insulin might be unreasonable,” adds D’souza.
Dhinagar says insulin is stored in health centres, “but we haven’t found a sustainable way to dispense them through mobile clinics yet.”
Cultural Factors and Misinformation Impeding Administration
The doctors say misinformation, superstition and lack of social support are also significant reasons insulin use and access suffer. “I remember a 16-year-old patient, Parvathy, who came to seek care from our centre,” recalls Singh. “Her abdomen was filled with branding marks because her relatives believed that she was possessed by a spirit which made her continuously sick. It was heartbreaking.”
Singh says many children who suffer from chronic diseases have been branded by their families in the belief that branding will banish evil spirits.
“It is difficult to explain to villagers what insulin is and why their body is not producing any. Their lack of basic understanding of their bodies is a barrier to education,” says D’souza
Adding to misinformation and a lack of true information is the fact that there is no way for the patients to access support groups. “Because Type 1 diabetes is a rare disease, the patients who seek care from us are … likely the only ones in their locality with this illness. This prevents them from interacting, learning from each other, and availing any social support,” says Singh. She’s currently treating around 20 children with Type 1 diabetes, all of them from remote areas who have never met each other.
Social Consequences of having Diabetes
In these patients, Type 1 diabetes has serious consequences. Most of them drop out of school because other students and teachers do not understand their disease, says Singh. They may have periods of prolonged absenteeism due to illness, which teachers do not understand and sometimes punish. They also feel shame at having to inject themselves at school. These things eventually lead to them becoming unemployable and not being able to live independently.
Availability and Affordability Challenges
While insulin vials and syringes are free at government centres in India, not all types of insulin might be available. For Type 1 diabetes, the ideal insulin regimens suggested are the basal-bolus and the split mixed regimen, which require a fast-acting insulin administered before meals and a slow-acting type of insulin that provides a steady effect throughout the day to maintain baseline blood sugar levels.
However, due to availability issues, the only option found in many government centres is human insulin, Mixtard, which combines a fast-acting and an intermediate-acting insulin in one vial, which Singh says does not control sugars well in Type 1 diabetes.
“We must also take note of the fact that pen devices and cartridges are expensive in India. Pen devices are easier to use and do not need refrigeration, which might make them an attractive option for patients. However, if patients have to pay for their insulin in this form, along with a glucometer and their strips, it would cost around 4,000 Indian rupees a month (approximately US$50), which is about half the monthly income of a rural Indian family. People then end up abandoning treatment when the cost burden increases,” Singh says.
A recent costing study by Médecins Sans Frontières, published in JAMA, the journal of the American Medical Association, in March 2024, reveals that a basal-bolus insulin regimen could be priced as low as US$96 (Rs 8500) a year using a reusable pen device and still generate profit for manufacturers. A prefilled long-acting insulin pen that could be sold at less than US$1 (Rs 88), is sold in India at around US$7.90(Rs 700). In the United States, this same pen costs US$28.40 (Rs 2516), at a markup of 2,153 per cent.
In a country like India, where more than 25 crore people survive on less than Rs 200 a day, this cost for a pen device also makes diabetes care increasingly inaccessible
Global Shifts in Manufacturing Priorities
Globally, the three corporations dominating insulin production and sales — Eli Lilly, Novo Nordisk and Sanofi — are moving away from producing insulin and focussing on GLP1 agonists such as Mounjaro and Ozempic. (Glucagon-like peptide-1 (GLP-1) agonists are a class of medications utilized to treat Type 2 Diabetes Mellitus (T2DM) and obesity.) These are injectable anti-diabetic agents that are currently also used for tackling weight loss and obesity. This trend emerged after the U.S. government compelled companies to reduce the prices of their insulin products by 70%, capping them at approximately US$30 (Rs 2658) per vial.
The projected loss of profit from insulin has led them to this shift of focus to more profit-generating GLP 1 agonists, with Novo Nordisk going so far as announcing that it will stop manufacturing insulin pen devices. This shift has already begun, causing issues in the developed world, where many diabetics in the U.S. and United Kingdom cannot access insulin because of supply issues.
The effects of this trend could be catastrophic in developing countries such as India, where insulin shortages would exacerbate existing barriers to access.
Unlike in wealthier countries, where patients might face affordability issues but generally have consistent access to health-care infrastructure, the obstacles in rural India are compounded by systemic inequities including limited infrastructure, inconsistent electricity and low levels of health literacy. This global shift could further diminish insulin supplies for communities already struggling to access the correct type of insulin due to cost and availability, leaving those most vulnerable at an even more significant disadvantage.
“In the developed world, pricing seems to be the main concern,” says D’souza. “But in the developing world, barriers to effectively using insulin include poor infrastructure, lack of electrification and limited health education. With these companies reducing insulin production, global supply issues will probably deepen our existing challenges, burdening families and health-care workers already fighting against difficult odds.”
After asking for help from many places, Singh was able to get free insulin pens and glucometers for her patients, sponsored by Life For A Child Australia, a not-for-profit organization focused on helping children with Type 1 diabetes.
Singh’s patients now get subsidised blood sugar monitoring and other blood tests and the care they need. “Back in the day, a Type 1 diabetes diagnosis in my centre would mean a death sentence for my patients, but now, we are slowly able to change the narrative,” she says.
There is an urgent need to address the systemic barriers to insulin access and ensure sustainable, equitable solutions that prioritize the health and well-being of all individuals living with diabetes.
This story was previously published in GenevaHealthFiles here
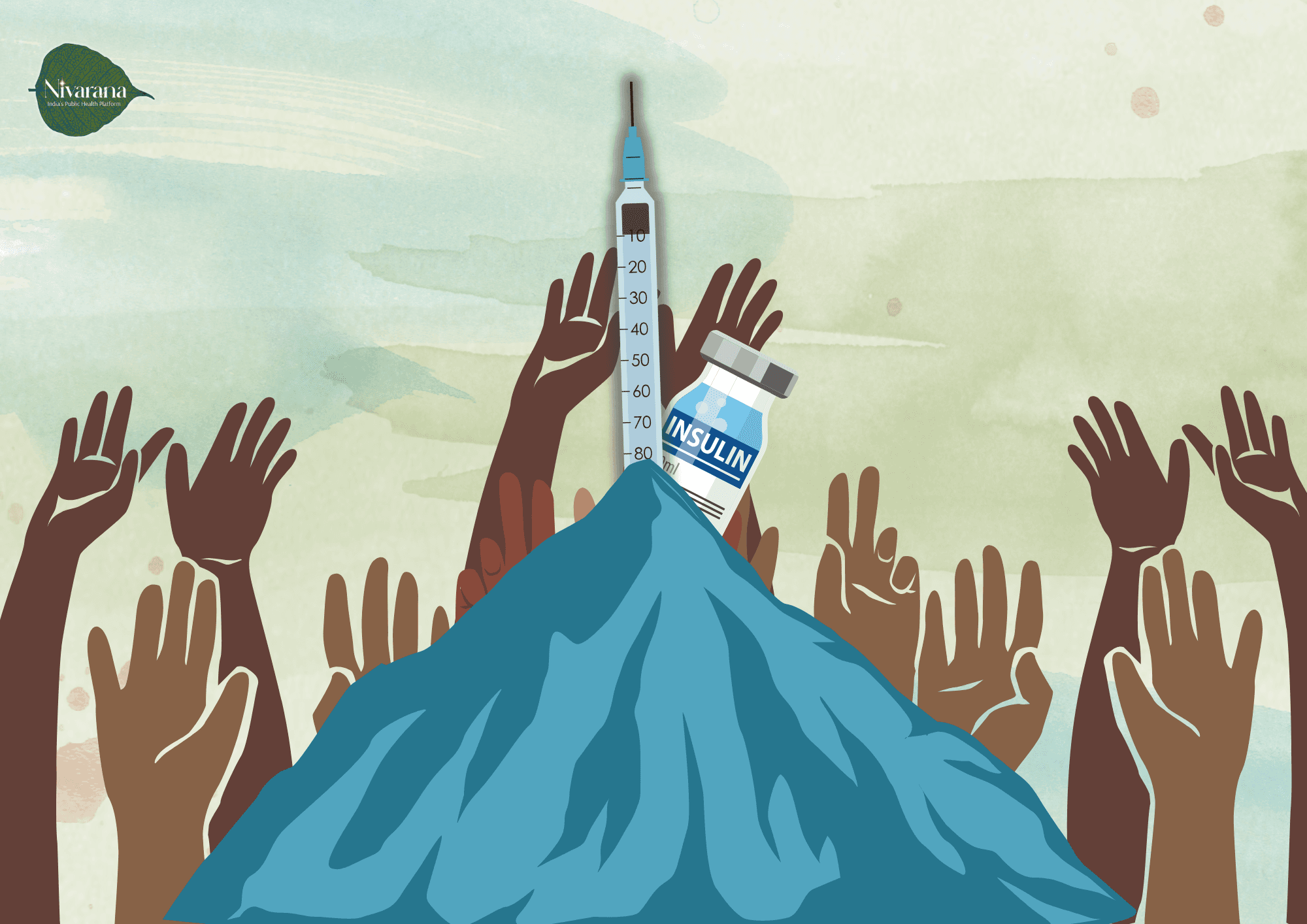
Image by Janvi Bokoliya