Swapan (name changed), a 63-year-old retired teacher from West Bengal, woke up at 5 am, freshened up, and called his buddy to go for a walk in the morning. He inhaled steam to get symptomatic relief from his chronic sinusitis. Walking the first 1km was hard as he experienced shortness of breath and a cough. The remaining 5km involved walking along the banks of the river. They ended their walk with a tea break and had a fun chit-chat session. He returned home after making a pitstop at the nearby market to buy groceries.
He lay down for a while, did household chores, took a bath, and cooked his meals. He ate his breakfast as usual before 10 am, his lunch between 1 pm and 3 pm, and spent the rest of his day with his smartphone. He ate his dinner by 6:45 pm as he does these days to make sure he is following his intermittent fasting schedule. He used to drink 150 ml of whiskey to help himself get to sleep early, and it was also a means to achieve pleasure.
Currently, he has stopped drinking alcohol for more than ten days.
But this healthy lifestyle was not always the case for Swapan.
He had lost his wife, who was also his best friend, to a stroke followed by Covid-19 and chronic kidney disease in 2023. During this stressful time, he developed hypertension and was started on anti-hypertensive medications. Losing his wife was a major life event. He lost his focus and was unable to concentrate on his daily habits of reading and writing.
But even before that, Swapan was the sole caregiver for his wife for three and a half years before her demise. During this period, stress and sadness made him lose about ten kilograms of weight. Only after her demise did he have some time to catch up on his meals and regain weight.
But he was unable to sleep. Grief flooded his mind. “What could I have done better to avoid my wife’s demise?” was a thought that kept occurring in circles.
Swapan was also a known patient of hypertension on medications for the same. On top of this and his grief, his 41-year-old habit of smoking, which was indispensable for him, had also begun to give him shortness of breath on exertion.
Swapan identified that he needed to make urgent lifestyle changes at this point, but he lacked the motivation or the information to be able to do so. His poor mental health compounded the difficulty he faced in doing anything to improve his health. And chronic disease care, as it exists in India, would not have been able to serve his needs and help him bring his disease under control.
No Awareness, Only Prescriptions
A hospital visit for non-communicable chronic conditions like hypertension or diabetes typically involves getting the patient to get a few blood tests, a prescription after diagnosis, and a follow-up visit in a few days. Quite often, patients leave the hospital without a clear understanding of the disease - how it affects their body, what things they need to look out for and other relevant information.
This is because the counselling provided in a few short doctor’s visits is not enough to establish robust foundational knowledge and understanding of their bodies and the disease in patients.
This lack of understanding leads to a gap in continuous care where NCDs(Non-communicable Diseases) thrive.
Continuous care is a term that refers to the ongoing, coordinated delivery of healthcare services to a patient over time, across different stages of illness, levels of care, and healthcare settings. Continuous care ensures that the patient receives appropriate care throughout his lifetime for his chronic illness and stays optimally protected against any complications or issues that arise from having that illness.
However, such care is a rarity in India.
A study in the West Bengal rural population showed that a total of 39.4% were not taking medications regularly, and 67.1% were unable to follow a healthy lifestyle and were not following up regularly with their healthcare providers.
This then means that they end up not noticing when their disease is worsening, which ultimately leads to emergencies, avoidable hospitalisations, and suffering. For example, Diabetic patients may not notice when they are beginning to have nerve damage in their feet due to the disease, but this will then lead to wounds and ulcers in the feet and carry a risk of losing the limb. Similarly, eye and kidney problems caused by diabetes may not be visible in their early stages, but lead to drastic problems such as kidney failure and loss of vision later.
To solve this, and to help patients become active participants in their own health, we use a model known as the User Driven Healthcare(UDHC) model, which aims to empower and partner with patients to help them take proactive measures to monitor and make critical decisions about their health.
Empowerment As A Treatment Plan
User-driven healthcare empowers patients and their caregivers with adequate knowledge about the diagnosis and the expected progression of the disease. It focuses on empowering them to look for early signs of progression of the disease before they become critical. This model uses health indicators that are easy to measure, such as checking blood pressure, glucose levels, etc, and empowers patients to make informed decisions about their lifestyle, nutrition, and daily activities.
Not only the patient, this model emphasizes the vital role of the advocate—a family member or a friend involved in the patient’s care journey. By empowering both patient and advocate, we take a collaborative approach to address the emotional, spiritual, and psychological needs of both.
This approach overcomes a key shortcoming of traditional healthcare systems—where advocates are often sidelined. We implement this by closing knowledge gaps and involving them in medical decision-making, which creates a vital safety net against harmful outcomes.
Swapan told his friends about his condition. One of his friends, who happens to be a volunteer working with User-Driven Health Care, introduced Swapan to the idea. A talk with him revealed that he is in need of help that moved beyond what the traditional healthcare system could do for him.
We decided to ask Swapan and his daughter, the patient advocate, whether they would be interested in being a part of a program where we attempted to realise User-Driven HealthCare. When they agreed, they were added to a PaJR (Patient Journey Record System) group on WhatsApp.
Patient Journey Record System(PaJR)
At KIMS Narketpally, we implement UDHC as a collaborative approach with the Patient Journey Record System. PaJR is an open-source collaborative framework that involves a network of healthcare professionals from various disciplines, translators to facilitate conversation in native languages, medical students, AI engineers, and most importantly, patients with similar disease patterns like type 1 diabetes, Kidney disease with varying etiologies, metabolic syndrome, etc, who help and support each other based on their real life experiences.
All of these diverse professionals and patients are part of WhatsApp groups known as PaJR groups for their specific diseases.
A patient whose lived experience with a disease is invaluable becomes a collaborator/caregiver for their peers with similar disease patterns. This forms a peer-support network of global collaborators from various fields (not limited to medical sciences) to improve outcomes of patients through evidence-based recommendations.
The PaJR came to be on the day humans started journaling their lives. All books, journals, biographies, and memoirs are medical case reports.
An interaction with a long-distance patient about 25 years ago, on an e-mail thread to follow up and improve their outcome, started a snowball effect.
We logged 5000 case reports in the last 5 years in the learning portfolios of medical students from various institutes. We are currently logging our PaJR case reports at pajrcasereporter.
With advancing internet and connectivity, we currently use accessible platforms like WhatsApp as a medium to stay connected with our patients and deliver continuous care from the point of first contact. PaJR enables us to make sure patients are taking their medicines regularly, adjust the dosage of medicines with prognosis, track vital parameters like BP, and blood sugar to identify shifts in trends for faster intervention and prevention of hospitalisation and suffering.
We believe that a patient-centric model like PaJR will democratize medical knowledge for the patient. A patient who learns more about their disease is empowered and asks for better quality healthcare. Our singular aim is to achieve that. PaJR not only democratizes knowledge to the patient, it also asks doctors to deliver better care to improve the care outcomes.
PaJR integrates telemedicine and Electronic Health Records (EHR) to keep track of the health and lifestyle data of the patient. It brings together patients and advocates with a global network of collaborators. It builds a detailed, long-term record of each patient, making it easier for doctors to share information when sending patients to higher-tier hospitals. These records containing information about daily lifestyle are being used to develop a semantic web, which will help Large Language Models(LLMs) to view patients as humans rather than clinical cases.
Swapan is one of our long-distance patients. He was admitted to our hospital for a general examination. From his symptoms of shortness of breath and some medical test reports, he was diagnosed with chronic obstructive pulmonary disease, heart disease, and controlled but variable blood pressure. A mental health evaluation also showed that he was suffering from an acute grief reaction and a sleep disorder.
Swapan knew it was going to be a boring task to write a log of his daily activities and send them to our PaJR group every day. Nonetheless, he is maintaining his streak for more than 9 months now - by logging every little detail meticulously, from the time he wakes up to the time he goes to bed. He doesn’t identify himself as a patient, but a collaborator who is trying to provide as much information as possible to help us analyse this data and achieve better outcomes.
Initially, he sent his blood pressure(BP) readings every hour during the day. He used to send >10 BP readings every day from morning to evening, once every hour (as mentioned in the image below). We slowly tapered his antihypertensive medicines. As his BP improved eventually, he sent BP readings once a day. Now, we are monitoring his BP every fortnight. We attribute his normal BP readings to his lifestyle changes - walking 6km every day, consuming a balanced diet, and intermittent fasting.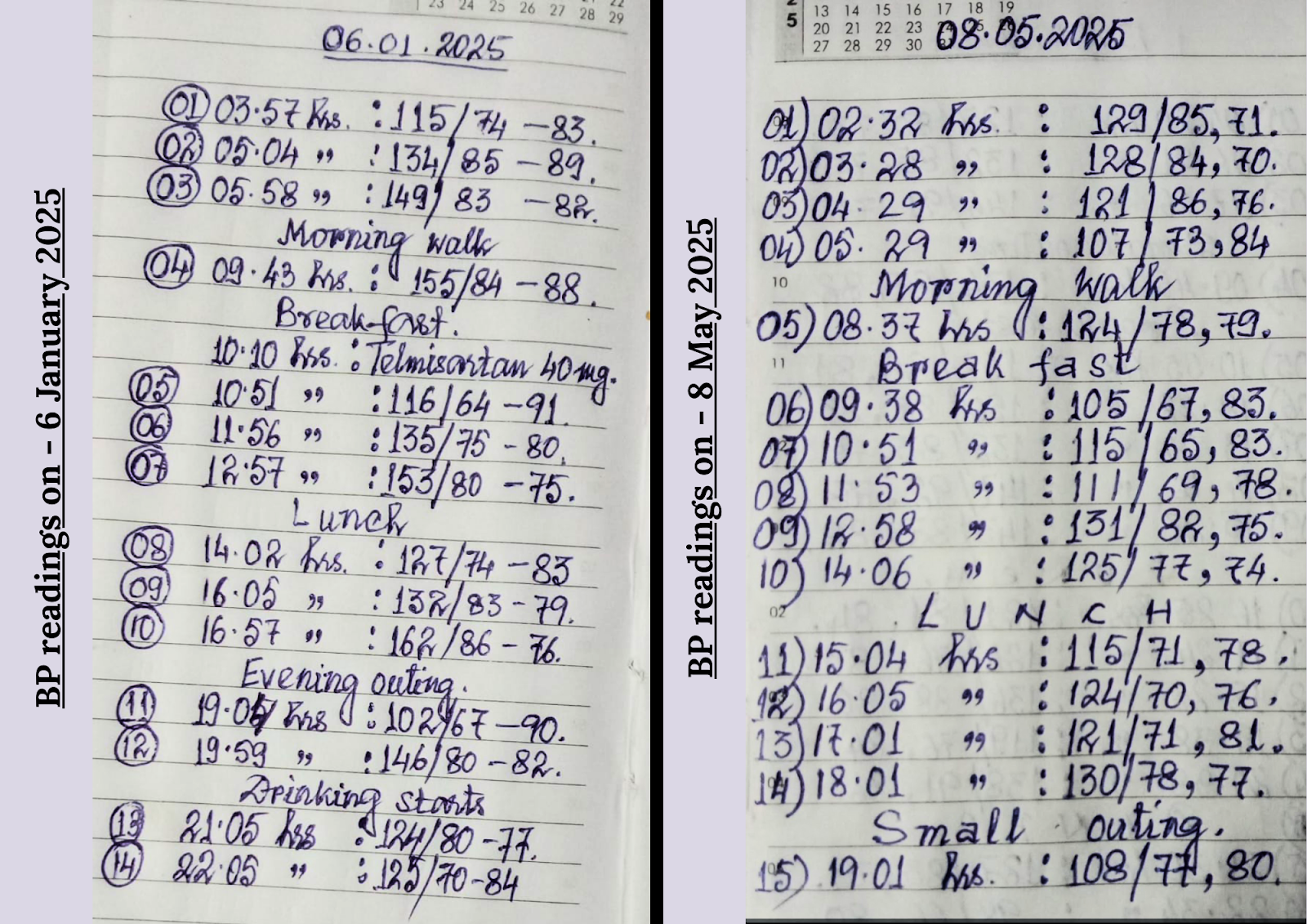
BP readings logged by Swapan.
He logs his habit of smoking, accounting for every single cigarette he smokes. He went from smoking 1.5 to 2 packs of cigarettes per day to 1 pack of cigarettes per day now. He logged the amount of alcohol he consumed every day until the day he quit.
He says, maintaining a log of his daily activities in a PaJR group gives him reassurance as his care team is well informed about him and his lifestyle, and would help the team in making better decisions for his health. He exercises well, eats well but still struggles to sleep and concentrate on reading and writing.
The Stories Of Transformation
The true success of this system is seeing the tangible joy and improved well-being of our patients.
In this patient-centric model, we measure outcomes against what the patients state as their goals, as well as other standardised PROs(Patient Related Outcomes). Patient goals might include lifestyle, mental health, and even personal goals like helping a patient prepare for exams. Patient-centric goals are shaped by what the patient values most, like recovery, symptom control, quality of life, or emotional support. Clinical outcomes are framed as disease-specific clinical complexity triads like concordance–complications–mortality in diabetes and metabolic syndrome complexities, and ascites–encephalopathy–diabetes in hypertension, which help us measure the severity of the illness.
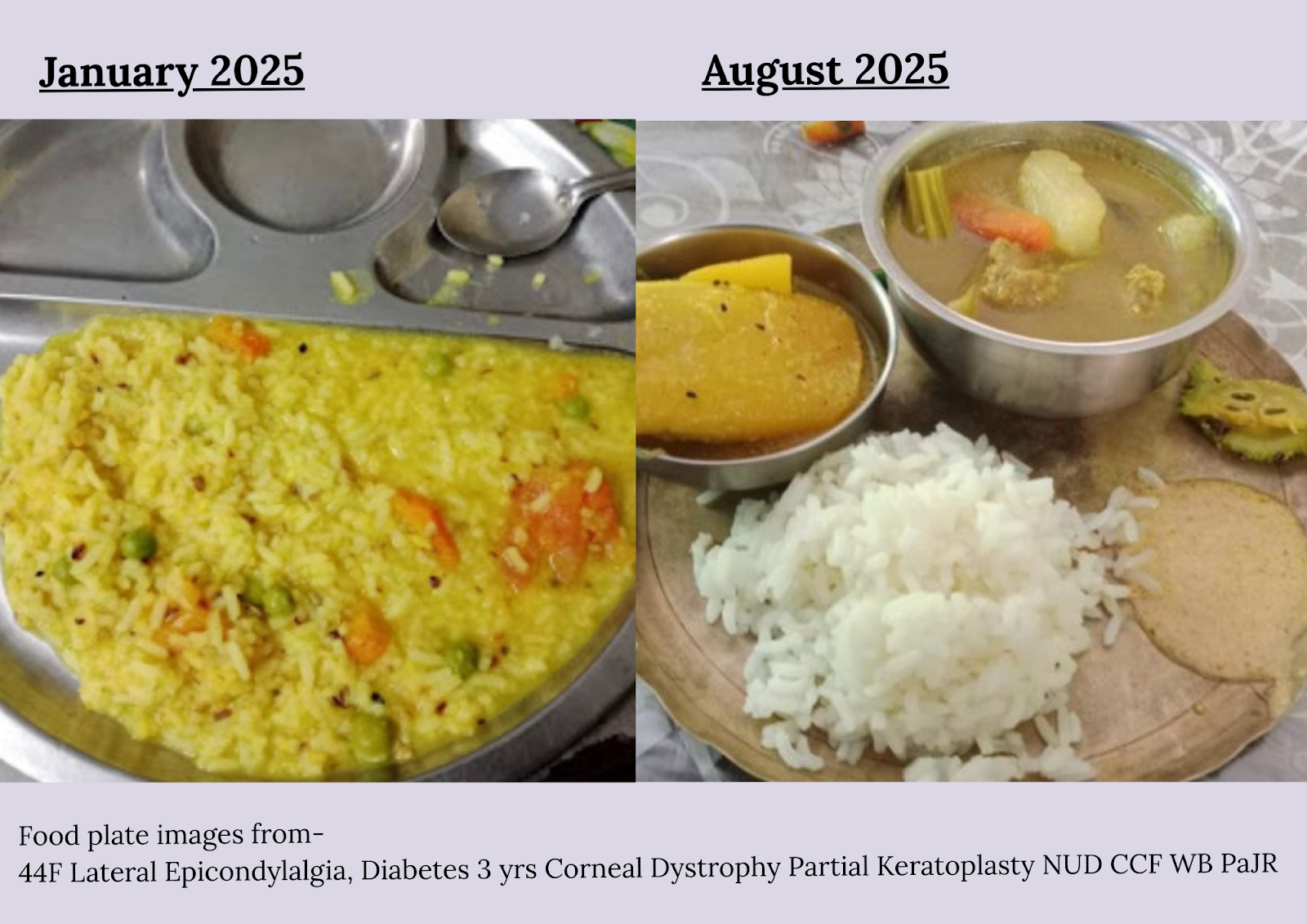
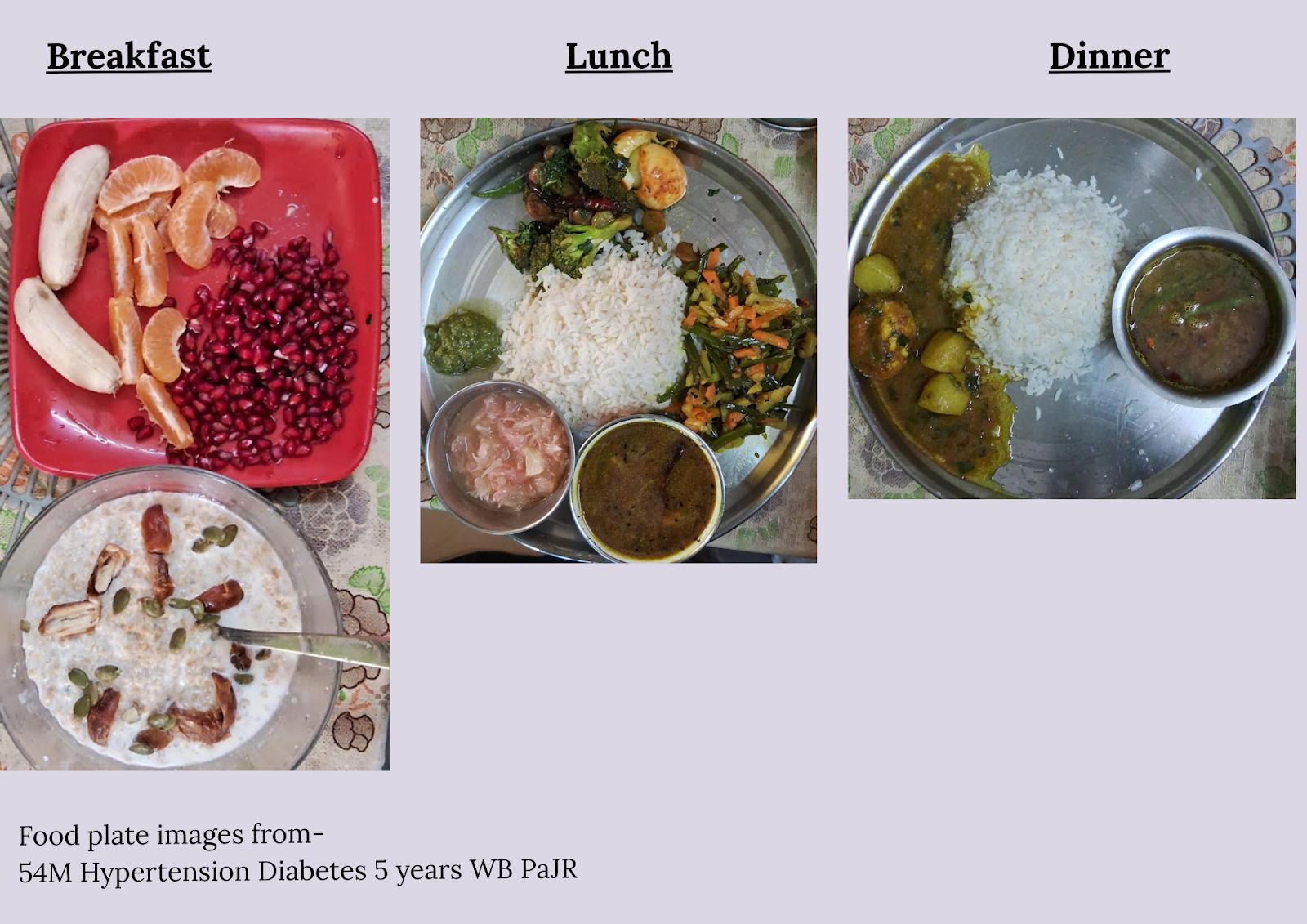
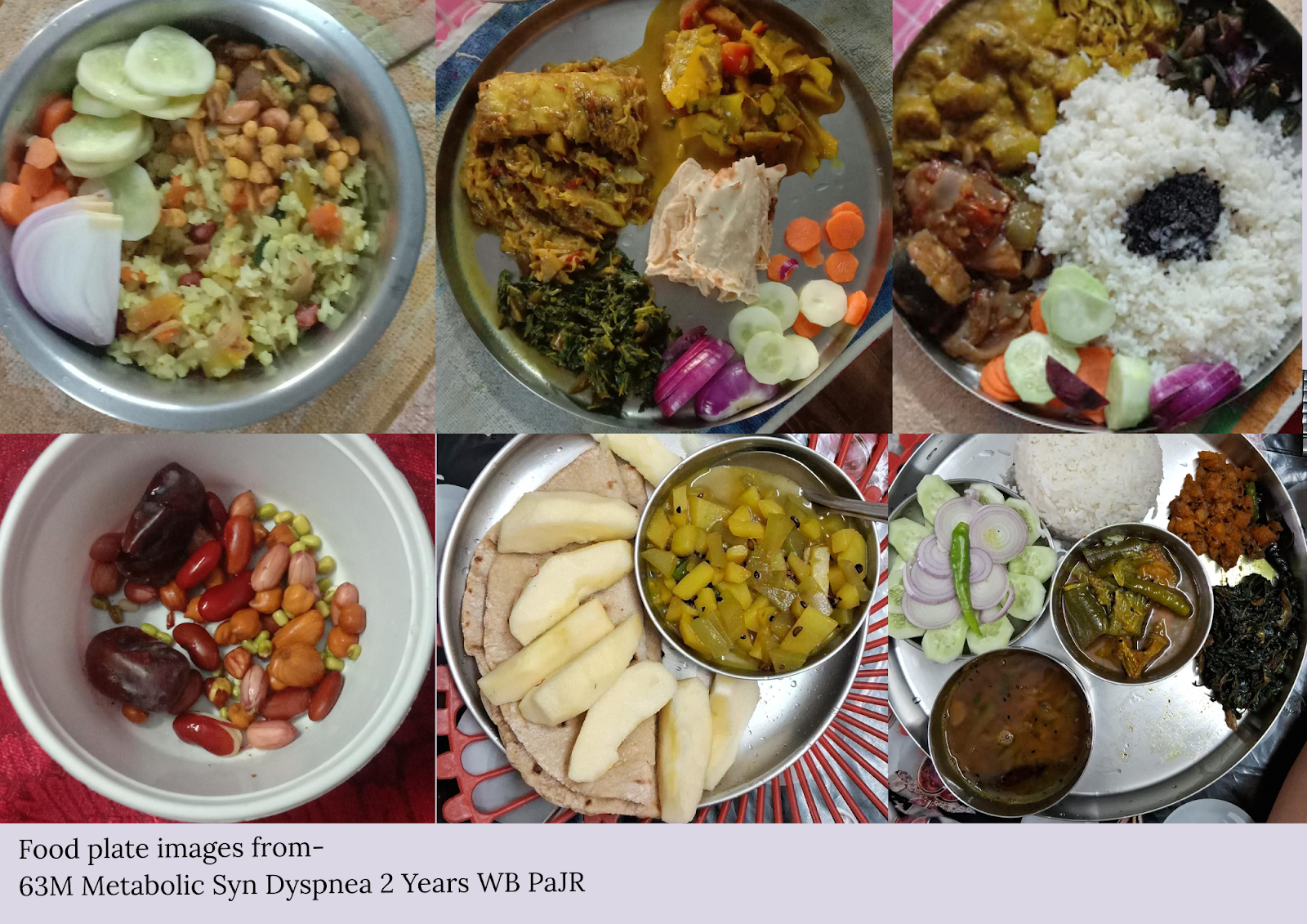
The best part of PaJR is the food plate photos of the meals shared by our patients, which transition from carb-rich food(mostly curry and rice) to a balanced diet (lower rice quantity with curry, fruits, and nuts) within days. Patients share a timestamped log of medications taken, the daily activities, and the amount of exercise they do every day, which helps in optimizing the pharmacotherapy by tapering and eventually adjusting the dose of medicines within a few months.
A hypertension patient told us about how walking 3 miles a day has elevated his mood and increased his productivity during work hours.
Some of the food plate images shared by our patients in PaJR groups. These transformations show us how they have shifted from a calorie rich diet to a balanced diet, eliminating a critical lifestyle risk factor of numerous NCDs.
We tracked pedal edema prognosis in a lupus nephritis patient on a PaJR group. This follow-up with the patient, spanning months, helped us in monitoring and reassuring the patient about the prognosis. We are still connected with the patient, and she is currently in remission.
Challenges and Learning
The current model requires patients to have a smartphone and basic digital skills. To bridge this, we make weekly phone calls to patients.
Volunteers are medical students from the institute, replaced by new students as they graduate. Some continue to follow up with their patients even after graduation; however, PaJR groups sometimes become inactive if patients are not proactive in sharing daily updates.
Furthermore, the volunteers are currently working for free, which is something that needs to be worked on in order to ensure the system does not get exploitative in the future.
The Way Forward
User-Driven HealthCare (UDHC) is an open-source project. We want to translate this successful UDHC model beyond our institution. This system can be a game-changer in tracking and modifying real-time behavioural and lifestyle changes in navigating patients’ illnesses remotely.
Swapan’s condition improved considerably after he received support from collaborators. His access to knowledge and the accountability he feels towards his group have considerably improved his lifestyle and healthcare outcomes. The lifestyle changes he could not implement with sheer willpower have become accessible to him via this support system.
Our hope is to be able to extend similar help to every patient and person who needs it.
Acknowledgements
I acknowledge the support and inputs of Dr. Rakesh Biswas, Dr. Aditya Samitinjay, Dr. Abdul Salam, Dr. Ayushi Tandon, Braahmani Bobba, and Mansi Agarwal for helping with drafting this article.
Sources to learn more about this project:
Websites: pajr.in , NarketpallySyndrome
Case report databases: MedicineDepartment, UDHC, PajrCaseReporter
Contact: deekshithvodela@gmail.com
Edited by Christianez Ratna Kiruba
Image by Christianez Ratna Kiruba